ADHD was first described by
Dr. Heinrich Hoffman in 1845. A physician who wrote books on medicine and psychiatry, Dr. Hoffman was also a poet who became
interested in writing for children when he couldn't find suitable materials to read to his 3-year-old son.
The result was a book of poems,
complete with illustrations, about children and their characteristics. "The Story of Fidgety Philip" was an accurate description
of a little boy who had attention deficit hyperactivity disorder. Yet it wasn't until 1902 that Sir George F. Still published a series of lectures to the Royal College of Physicians
in England in which he described a group of impulsive children with significant behavioral problems, caused by a genetic dysfunction
and not by poor child rearing, children who today would be easily recognized as having ADHD.1
Since then, several thousand
scientific papers on the disorder have been published, providing information on its nature, course, causes, impairments and
treatments.
A child with ADHD faces a
difficult but not insurmountable task ahead. In order to achieve his or her full potential, he or she should receive help,
guidance and understanding from parents, guidance counselors and the public education system. Following is information on ADHD and its management,
including research on medications and behavioral interventions, as well as helpful resources on educational options.
 
Is It Really ADHD?
Not everyone who is overly
hyperactive, inattentive or impulsive has ADHD. Since most people sometimes blurt out things
they didn't mean to say, or jump from one task to another or become disorganized and forgetful, how can specialists tell if
the problem is ADHD?
Because everyone shows some
of these behaviors at times, the diagnosis requires that such behavior be demonstrated to a degree that's inappropriate for
the person's age. The diagnostic guidelines also contain specific requirements for determining when the symptoms indicate
ADHD.
The behaviors
must appear early in life, before age 7 and continue for at least 6 months. Above
all, the behaviors must create a real handicap in at least 2 areas of a person's life such as:
- in the schoolroom
- on the playground
- at home
- in the community
- in social settings
So someone who shows some
symptoms but whose schoolwork or friendships aren't impaired by these behaviors wouldn't be diagnosed with ADHD. Nor would a child who seems overly active on the playground but functions well elsewhere receive an ADHD diagnosis.
To assess whether a child
has ADHD, specialists consider several critical questions:
- Are these behaviors excessive, long-term and pervasive? That
is, do they occur more often than in other children the same age?
- Are they a continuous problem, not just
a response to a temporary situation?
- Do the behaviors occur in several settings or only in one specific
place like the playground or in the schoolroom?
The person's pattern of behavior
is compared against a set of criteria and characteristics of the disorder as listed in the DSM-IV-TR.

Diagnosis
Some parents see signs of
inattention, hyperactivity and impulsivity
in their toddler long before the child enters school. The child may lose interest in playing a game or watching a TV show
or may run around completely out of control.
But because children mature
at different rates and are very different in personality, temperament and energy levels, it's useful to get an expert's opinion of whether the behavior is appropriate for the child's age.
Parents can ask their child's
pediatrician, or a child psychologist or psychiatrist, to assess whether their toddler has an attention
deficit hyperactivity disorder or is, more likely at this age, just immature or unusually exuberant.
ADHD may be suspected by a
parent or caretaker or may go unnoticed until the child runs into problems at school. Given that ADHD
tends to affect functioning most strongly in school, sometimes the teacher is the first to recognize that a child is hyperactive or inattentive and may point it out to the parents &/or consult
with the school psychologist.

Because teachers work with
many children, they come to know how "average" children behave in learning situations that require attention and self-control.
However, teachers sometimes fail to notice the needs of children who may be more inattentive and passive yet who are quiet
and cooperative, such as those with the predominantly inattentive form of ADHD.
Professionals Who Make the
Diagnosis.
If ADHD
is suspected, to whom can the family turn? What kinds of specialists do they need?
Ideally, the diagnosis should
be made by a professional in your area w/training in ADHD or in the diagnosis of mental
disorders. Child psychiatrists and psychologists, developmental / behavioral pediatricians or behavioral neurologists are
those most often trained in differential diagnosis. Clinical social workers may also have such training.
The family can start by talking
with the child's pediatrician or their family doctor. Some pediatricians may do the assessment themselves, but often they
refer the family to an appropriate mental health specialist they know and trust.
In addition, state and local
agencies that serve families and children, as well as some of the volunteer organizations listed at the end of this document,
can help identify appropriate specialists.

| Specialty |
Can Diagnose ADHD |
Can prescribe medication, if needed |
Provides counseling or training |
| Psychiatrists |
yes |
yes |
yes |
| Psychologists |
yes |
no |
yes |
| Pediatricians or Family Physicians |
yes |
yes |
no |
| Neurologists |
yes |
yes |
no |
| Clinical Social workers |
yes |
no |
yes |
 
Knowing the differences in
qualifications and services can help the family choose someone who can best meet their needs. There are several types of specialists
qualified to diagnose and treat ADHD.
Child psychiatrists are doctors
who specialize in diagnosing and treating childhood mental and behavioral disorders. A psychiatrist can provide therapy and
prescribe any needed medications. Child psychologists are also qualified to diagnose and treat ADHD.
They can provide therapy for
the child and help the family develop ways to deal with the disorder. But psychologists aren't medical doctors and must rely
on the child's physician to do medical exams and prescribe medication.
Neurologists, doctors who
work with disorders of the brain and nervous system, can also diagnose ADHD and prescribe
medicines. But unlike psychiatrists and psychologists, neurologists usually don't provide therapy for the emotional aspects
of the disorder.

Within each specialty, individual
doctors and mental health professionals differ in their experiences with ADHD. So in selecting
a specialist, it's important to find someone with specific training and experience in diagnosing and treating the disorder.
Whatever the specialist's
expertise, his or her first task is to gather information that will rule out other possible reasons for the child's behavior.
Among possible causes of ADHD-like behavior are the following:
- A sudden change in the child's life: the death of a parent or grandparent; parents' divorce; a parent's job loss
- Undetected seizures, such as in petit mal or temporal lobe
seizures
- A middle ear infection that causes intermittent hearing problems
- Medical disorders that may affect brain functioning
- Under-achievement caused by learning disability
- Anxiety or depression.

Ideally, in ruling out other
causes, the specialist checks the child's school & medical records. There may be a school record of hearing or vision
problems, since most schools automatically screen for these.
The specialist tries to determine
whether the home & classroom environments are unusually stressful or chaotic & how the child's parents & teachers deal w/the child.
Next the specialist gathers
information on the child's ongoing behavior in order to compare these behaviors to the symptoms & diagnostic criteria
listed in the DSM-IV-TR. This also involves talking w/the child & if possible, observing the child in class & other settings.
The child's teachers, past
& present, are asked to rate their observations of the child's behavior on standardized evaluation forms, known as behavior
rating scales, to compare the child's behavior to that of other children the same age.

While rating scales might
seem overly subjective, teachers often get to know so many children that their judgment of how a child compares to others
is usually a reliable & valid measure.
The specialist interviews
the child's teachers & parents & may contact other people who know the child well, such as coaches or baby-sitters.
Parents are asked to describe their child's behavior in a variety of situations. They may also fill out a rating scale to
indicate how severe & frequent the behaviors seem to be.
In most cases, the child will
be evaluated for social adjustment & mental health. Tests of intelligence & learning achievement may be given to see
if the child has a learning disability & whether the disability is in one or more subjects.
In looking at the results
of these various sources of information, the specialist pays special attention to the child's behavior
during situations that are the most demanding of self-control, as well as noisy or unstructured situations such as
parties, or during tasks that require sustained attention, like reading, working math problems or playing a board game.

Behavior during free play
or while getting individual attention is given less importance in the evaluation. In such situations, most children w/ADHD are able to control their behavior & perform better than in more restrictive situations.
The specialist then pieces
together a profile of the child's behavior. Which ADHD-like behaviors listed in the most
recent DSM does the child show?
- How often?
- In what situations?
- How long has the child been doing them?
- How old was the child when the problem started?
- Are the behavior problems relatively chronic or enduring or
are they periodic in nature?
- Are the behaviors seriously interfering w/the child's friendships,
school activities, home life, or participation in community activities?
- Does the child have any other related problems?

The answers to these questions
help identify whether the child's hyperactivity, impulsivity
& inattention are significant & long-standing. If so, the child may be diagnosed
w/ADHD.
A correct diagnosis often
resolves confusion about the reasons for the child's problems that lets parents & child move
forward in their lives w/more accurate information on what's wrong & what can be done to help.
Once the disorder is diagnosed,
the child & family can begin to receive whatever combination of educational, medical & emotional help they need. This
may include providing recommendations to school staff, seeking out a
more appropriate classroom setting, selecting the right medication & helping parents to manage their child's behavior.
 
What Causes ADHD?
One of the first questions
a parent will have is "Why? What went wrong?" "Did I do something to cause this?"
There's little compelling
evidence at this time that ADHD can arise purely from social factors or child-rearing methods.
Most substantiated causes appear to fall in the realm of neurobiology & genetics.
This isn't to say that environmental factors may not influence the severity of the disorder & especially the degree of impairment & suffering the child may experience, but
that such factors don't seem to give rise to the condition by themselves.
The parents' focus should
be on looking forward & finding the best possible way to help their child. Scientists are studying causes in an effort
to identify better ways to treat & perhaps someday, to prevent ADHD.
They're finding more &
more evidence that ADHD doesn't stem from the home environment, but from biological causes.
Knowing this can remove a huge burden of guilt from parents who might blame themselves for their
child's behavior.
Over the last few decades,
scientists have come up w/possible theories about what causes ADHD. Some of these theories
have led to dead ends, some to exciting new avenues of investigation.

Environmental Agents
Studies have shown a possible correlation between the use of cigarettes & alcohol during pregnancy & risk for ADHD in the offspring of that pregnancy. As a precaution, it's best during pregnancy to refrain from both cigarette
& alcohol use.
Another environmental agent
that may be associated w/a higher risk of ADHD is high levels
of lead in the bodies of young preschool children.
Since lead is no longer allowed
in paint & is usually found only in older buildings, exposure to toxic levels isn't as prevalent as it once was. Children who live in old buildings in which lead still exists in the plumbing or in lead paint
that has been painted over may be at risk.
Brain Injury
One early theory was that
attention disorders were caused by brain injury. Some children who've suffered accidents leading to brain injury may show
some signs of behavior similar to that of ADHD, but only a small percentage of children
w/ADHD have been found to have suffered a traumatic brain injury.

Food Additives & Sugar
It's been suggested
that attention disorders are caused by refined sugar or food additives, or that symptoms
of ADHD are exacerbated by sugar or food additives.
In 1982, the National
Institutes of Health held a scientific consensus conference to discuss this issue. It was found that diet restrictions helped
about 5% of children w/ADHD, mostly young children who had food allergies.3
A more recent
study on the effect of sugar on children, using sugar one day & a sugar substitute on alternate days, w/out parents, staff,
or children knowing which substance was being used, showed no significant effects of the sugar
on behavior or learning.4
In another study,
children whose mothers felt they were sugar-sensitive were given aspartame as a substitute for sugar. Half the mothers were
told their children were given sugar, half that their children were given aspartame.
The mothers who
thought their children had received sugar rated them as more hyperactive than the other children & were more critical of their behavior.5

Genetics
Attention disorders often run in families, so there are likely to be genetic influences.
Studies indicate that 25% of the close relatives in the families of ADHD children also have
ADHD, whereas the rate is about 5% in the general population.6 Many studies of twins now show that a strong genetic influence exists in the disorder.7
Researchers continue
to study the genetic contribution to ADHD & to identify the genes that cause a person
to be susceptible to ADHD. Since its inception in 1999, the Attention-Deficit Hyperactivity
Disorder Molecular Genetics Network has served as a way for researchers to share findings regarding possible genetic influences
on ADHD.8
Recent Studies on Causes of ADHD
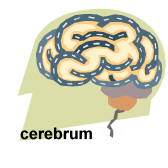
Some knowledge of the structure
of the brain is helpful in understanding the research scientists are doing in searching for a physical basis for attention deficit hyperactivity disorder. One part of the brain that scientists have focused on in their search
is the frontal lobes of the cerebrum.
 
The frontal lobes allow us
to solve problems, plan ahead, understand the behavior of others & restrain our impulses.
The two frontal lobes, the right & the left, communicate w/each other thru the corpus callosum,
(nerve fibers that connect the right & left frontal lobes).
The basal
ganglia are the interconnected gray masses deep in the cerebral hemisphere that serve as the connection between the
cerebrum & the cerebellum & w/the cerebellum,
are responsible for motor coordination. The cerebellum is divided
into 3 parts. The middle part is called the vermis.
All of these parts of the
brain have been studied thru the use of various methods for seeing into or imaging the brain. These methods include functional
magnetic resonance imaging (fMRI) positron emission tomography (PET) & single photon emission computed tomography (SPECT).
The main or central psychological
deficits in those w/ADHD have been linked thru these studies.

By 2002 the researchers in
the NIMH Child Psychiatry Branch had studied 152 boys & girls w/ADHD, matched w/139
age & gender -matched controls w/out ADHD.
The children were scanned
at least twice, some as many as 4 times over a decade. As
a group, the ADHD children showed 3-4% smaller brain volumes
in all regions - the frontal lobes, temporal gray matter, caudate nucleus & cerebellum.
This study also
showed that the ADHD children who were on medication had a white matter volume that didn't
differ from that of controls. Those never-medicated patients had an abnormally small volume of
white matter. The white matter consists of fibers that establish long-distance connections between brain regions. It
normally thickens as a child grows older & the brain matures.9
Although this long-term study
used MRI to scan the children's brains, the researchers stressed that MRI remains a research tool & can't be used to diagnose
ADHD in any given child. This is true for other neurological methods of evaluating the brain,
such as PET & SPECT.
 
The Treatment of ADHD
Every family wants to determine
what treatment will be most effective for their child. This question needs to be answered by each family in consultation w/their
health care professional. To help families make this important decision, the National Institute of Mental Health (NIMH) has
funded many studies of treatments for ADHD & has conducted the most intensive study
ever undertaken for evaluating the treatment of this disorder.
This study is known as the
Multimodal Treatment Study of Children w/ Attention Deficit Hyperactivity Disorder (MTA).12 The NIMH is now conducting a clinical trial for younger children ages 3 to 5.5 years (Treatment
of ADHD in Preschool-Age Children).
The Multimodal Treatment Study of Children with Attention Deficit
Hyperactivity Disorder.

The MTA study included 579
(95-98 at each of 6 treatment sites) elementary school boys & girls w/ADHD, who were randomly assigned to one of 4 treatment programs:
- (1) medication management
alone
- (2) behavioral treatment
alone
- (3) a combination of both
- (4) routine community care
In each of the study sites,
3 groups were treated for the first 14 months in a specified protocol & the 4th group was referred for community treatment
of the parents' choosing.
All of the children were reassessed
regularly throughout the study period. An essential part of the program was the cooperation of
the schools, including principals & teachers. Both teachers & parents rated the children on hyperactivity, impulsivity & inattention
& symptoms of anxiety & depression, as well as social skills.

The children in two groups
(medication management alone & the combination treatment) were seen monthly for 1/2
hour at each medication visit. During the treatment visits, the prescribing physician:
- spoke w/the parent
- met w/the child
- sought to determine any concerns that the family might have
regarding the medication or the child's ADHD-related difficulties
The physicians, in addition,
sought input from the teachers on a monthly basis. The physicians in the medication - only group didn't provide behavioral
therapy but did advise the parents when necessary concerning any problems the child might have.
In the behavior treatment-only
group, families met up to 35 times w/a behavior therapist, mostly in group sessions. These therapists also made repeated visits
to schools to consult w/children's teachers & to supervise a special aide assigned to each child in the group.

In addition, children attended
a special 8-week summer treatment program where they worked on academic, social & sports skills & where intensive behavioral therapy was delivered to assist children in improving their behavior.
Children in the combined therapy
group received both treatments, that is, all the same assistance that the medication-only received, as well as all of the
behavior therapy treatments.
In routine community care,
the children saw the community-treatment doctor of their parents' choice 1 to 2 times per year for short periods of time.
Also, the community-treatment doctor didn't have any interaction w/the teachers.
The results of the study indicated
that long-term combination treatments & the medication-management alone were superior
to intensive behavioral treatment & routine community treatment.

And in some areas, anxiety, academic performance, oppositionality, parent-child relations & social skills; the combined treatment was usually superior. Another advantage of combined treatment was that children could be successfully
treated w/lower doses of medicine, compared w/the medication-only group.
Treatment of Attention Deficit Hyperactivity
Disorder in Preschool-Age Children (PATS).
Because many children in the
preschool years are diagnosed w/ ADHD & are given medication, it's important to know
the safety & efficacy of such treatment.
The NIMH is sponsoring an ongoing multi-site study, "Preschool
ADHD Treatment Study" (PATS). It's the first major effort to examine the safety & efficacy
of a stimulant, methylphenidate, for ADHD in this age group.

The PATS study uses a randomized,
placebo-controlled, double-blind design. Children ages 3 to 5 who have severe & persistent symptoms of ADHD that impair their functioning are eligible for this study.
To avoid using medications
at such an early age, all children who enter the study are first treated w/behavioral therapy. Only children who don't show sufficient improvement w/behavior therapy are considered for the medication part of the study.
The study is being conducted
at New York State Psychiatric Institute, Duke University, Johns Hopkins University, New York University, the University of
California at Los Angeles & the University of California at Irvine. Enrollment in the study will total 165 children.
Which Treatment Should My Child Have?

For children w/ADHD, no single treatment is the answer for every child. A child may sometimes have undesirable side effects
to a medication that would make that particular treatment unacceptable.
And if a child w/ADHD also has anxiety or depression, a treatment combining medication & behavioral therapy might be best.
Each child's needs & personal history must be carefully considered.
Medications
For decades, medications have
been used to treat the symptoms of ADHD.
The medications that seem
to be the most effective are a class of drugs known as stimulants. Following is a list of
the stimulants, their trade (or brand) names & their
generic names. "Approved age" means that the drug has been tested & found safe & effective in children of that age.

| Trade Name |
Generic Name |
Approved Age |
| Adderall |
amphetamine |
3 and older |
| Concerta |
methylphenidate
(long acting) |
6 and older |
| Cylert* |
pemoline |
6 and older |
| Dexedrine |
dextroamphetamine |
3 and older |
| Dextrostat |
dextroamphetamine |
3 and older |
| Focalin |
dexmethylphenidate |
6 and older |
| Metadate ER |
methylphenidate
(extended release) |
6 and older |
| Metadate CD |
methylphenidate
(extended release) |
6 and older |
| Ritalin |
methylphenidate |
6 and older |
| Ritalin SR |
methylphenidate
(extended release) |
6 and older |
| Ritalin LA |
methylphenidate
(long acting) |
6 and older |
| *Because of its potential for serious side effects
affecting the liver, Cylert should not ordinarily be considered as first-line drug therapy for ADHD. |
The U.S. Food and Drug Adminstration (FDA) recently approved
a medication for ADHD that isn't a stimulant. The medication, Strattera®, or atomoxetine, works on the neurotransmitter norepinephrine,
whereas the stimulants primarily work on dopamine. Both of theses neurotransmitters are believed to play a role in ADHD. More
studies will need to be done to contrast Strattera w/the medications already available, but the evidence to date indicates
that over 70% of children w/ADHD given Strattera manifest significant improvement in their symptoms.
 
Some people get better results
from one medication, some from another. It's important to work w/the prescribing physician to find the right medication &
the right dosage. For many people, the stimulants dramatically reduce their hyperactivity
& impulsivity & improve their ability to focus,
work & learn.
The medications may also improve physical coordination, such as that needed in handwriting & in sports.
The stimulant
drugs, when used w/medical supervision, are usually considered quite safe. Stimulants don't make the child feel "high," although
some children say they feel different or funny. Such changes are usually very minor. Although some parents worry that their
child may become addicted to the medication, to date there's no convincing evidence that stimulant
medications, when used for treatment of ADHD, cause drug abuse or dependence.

A review of all
long-term studies on stimulant medication & substance abuse, conducted by researchers at Massachusetts General Hospital
& Harvard Medical School, found that teenagers w/ADHD who remained on their medication during the teen years
had a lower likelihood of substance use or abuse than did ADHD
adolescents who weren't taking medications.13
The stimulant drugs come in
long & short-term forms. The newer sustained-release stimulants can be taken before school & are long-lasting so that
the child doesn't need to go to the school nurse every day for a pill.
The doctor can discuss w/the
parents the child's needs & decide which preparation to use & whether the child needs to take the medicine during
school hours only or in the evening & on weekends too.
If the child doesn't show
symptom improvement after taking a medication for a week, the doctor may try adjusting the dosage. If there's still no improvement,
the child may be switched to another medication. About 1 out of 10 children isn't helped by a stimulant medication.
Other types of medication may be used if stimulants don't work or if the ADHD occurs w/another
disorder. Antidepressants & other medications can help control accompanying depression or anxiety.

Sometimes the doctor may prescribe
for a young child a medication that has been approved by the FDA for use in adults or older children. This use of the medication
is called "off label." Many of the newer medications that are proving helpful for child
mental disorders are prescribed off label because only a few of them have been systematically
studied for safety & efficacy in children.
Medications that haven't undergone
such testing are dispensed w/ the statement that "safety & efficacy haven't been established
in pediatric patients."
Side Effects of the Medications
Most side effects of the stimulant
medications are minor & are usually related to the dosage of the medication being taken. Higher doses produce more side
effects. The most common side effects are:

- decreased appetite
- insomnia
- increased anxiety &/or irritability
- some children report mild stomach aches or headaches
Appetite seems to fluctuate,
usually being low during the middle of the day & more normal by suppertime. Adequate amounts of food that is nutritional
should be available for the child, especially at peak appetite times.
If the child has difficulty
falling asleep, several options may be tried; a lower dosage of the stimulant, giving the stimulant earlier in the day, discontinuing
the afternoon or evening dosage, or giving an adjunct medication such as a low-dosage antidepressant or clonidine.
A few children develop tics
during treatment. These can often be lessened by changing the medication dosage. A very few children can't tolerate any stimulant,
no matter how low the dosage. In such cases, the child is often given an antidepressant instead of the stimulant.

When a child's schoolwork
and behavior improve soon after starting medication, the child, parents and teachers tend to applaud the drug for causing the sudden changes. Unfortunately, when people see
such immediate improvement, they often think medication is all that's needed.
But medications don't cure ADHD; they only control the symptoms on the day they're taken. Although the medications help the child pay better attention and complete school work, they can't increase knowledge or improve academic skills. The
medications help the child to use those skills he or she already possesses.
Behavioral therapy, emotional counseling and practical support will help ADHD children cope with everyday problems and feel better
about themselves.
Facts to Remember About Medication for ADHD
- Medications for ADHD help many children focus and be more successful at school, home and play. Avoiding
negative experiences now may actually help prevent addictions and other emotional problems later.
- About 80% of children who need medication for ADHD still need it as teenagers. Over 50% need medication as adults.
Medication for the Child with Both ADHD and Bipolar Disorder
Since a child with bipolar disorder will probably be prescribed a mood stabilizer such as lithium or Depakote®, the doctor will carefully consider whether the
child should take one of the medications usually prescribed for ADHD. If a stimulant medication is prescribed, it may be given in a lower dosage than usual.


another source never hurts
anything....
What is ADHD (Attention Deficit Hyperactivity Disorder)?
Health experts say that
ADHD (attention deficit hyperactivity disorder) is the most common behavioral
disorder that starts during childhood. However, it does not only affect children - people of all ages can suffer from ADHD.
Psychiatrists say ADHD is a neurobehavioral developmental disorder.
An individual with ADHD
finds it much more difficult to focus on something without being distracted. He has greater difficulty in controlling what
he is doing or saying and is less able to control how much physical activity is appropriate for a particular situation compared
to somebody without ADHD. In other words, a person with ADHD is much more impulsive and restless.
Health care professionals
may use any of the following terms when describing a child (or an older person)
who is overactive and has difficulty concentrating - attention deficit, attention deficit hyperactivity disorder, hyperkinetic
disorder, hyperactivity.
North Americans commonly
use the terms ADD (attention deficit disorder) or ADHD (attention deficit hyperactivity disorder). In the UK hyperkinetic disorder is the official term - however,
ADD and ADHD have become widely used.
ADHD in children is completely
different from normal childhood excited and boisterous behavior. Many children, especially very young ones, are inattentive
and restless without necessarily being affected by ADHD.
The Centers for Disease Control
and Prevention (CDC) estimates that approximately 4.4 million children aged 4 to 17 have been diagnosed with ADHD in the USA
by a healthcare professional. As of 2003 2 1/2 million American children aged 4 to 17 are being treated for ADHD with medicines.
The CDC adds that in 2003 7.8% of all school-aged American children were reported to have an ADHD diagnosis by their parent.

Three types of ADHD
According to the CDC, there are three types of ADHD. They are
defined according to which symptoms stand out the most.
- Predominantly
Inattentive Type
The person finds it very difficult to organize or finish a task. They find it hard to pay attention
to details and find it difficult to follow instructions or conversations.
- Predominantly
Hyperactive-Impulsive Type
The person finds it hard to keep still - they fidget and talk a lot. A smaller child
may be continually jumping, running or climbing. They are:
- restless and impulsive
- interrupting others
- grabbing things
- speaking at inappropriate
times
- They have difficulty
waiting their turn and find it hard to listen to directions. A person with this type of ADHD will have more injuries and/or
accidents than others.
- Combined Type
A
person whose symptoms include all those of 1 and 2, and whose symptoms are equally predominant. In other words, all the symptoms
in 1 and 2 stand out equally.
What are the
general signs of ADHD in children?
- the child is restless, overactive, fidgety
- the child is constantly chattering
- the child is continuously interrupting people
- the child cannot concentrate for long on specific tasks
- the child is inattentive
- the child finds it hard to wait his/her turn in play, conversations
or standing in line (queue)
The above signs may be observed in children frequently and usually
do not mean the child has ADHD. It is when these signs become significantly more pronounced in one child, compared to other
children of the same age, and when his/her behavior undermines his/her school and social life, that the child may have ADHD.
What causes ADHD?
We are not sure. Studies reveal that a person's risk of developing
ADHD is higher if a close relative also has/had it. Twin studies have indicated that ADHD is highly heritable. We also know
that ADHD is much more common in boys than girls. The scientific community generally agrees that ADHD is biological in nature.
Many reputable scientists believe ADHD is the result of chemical imbalances in the brain.
Some studies have indicated that food additives, specifically
some colorings, may have an impact on ADHD behaviors. In July 2008, the European Union ruled that synthetic food colorings
(called azo dyes) must be labeled not only with the relevant E number, but also with the words "may have an adverse effect
on activity and attention in children".
A 1984 study by Benton and team, demonstrated that sugar has no effect on behavior. A study in
1986 by Milich and Pelham, and another by Wolraich and team in 1985, also found no link between sucrose (sugar) and behavior
impact on children with ADHD. However, most sugars found in sugary foods and sweets (candy) consumed by children are corn
syrup and high fructose corn syrup - these sugars were not used in any of the above-mentioned studies.
Interesting link
Possible causes of ADHD (New Zealand's ADHD Online Support Group)
How do I know if I, my child, spouse
or relative has ADHD?
ADHD cannot be diagnosed physically, i.e. with a blood test,
urine test, brain scan or a physical check up. As most children have problems with self-control anyway, a proper diagnosis
can be quite challenging.
An ADHD diagnosis has to be carried out by a specialist - usually
a psychiatrist, psychologist or pediatrician. The specialist will observe the child and recognize behavior patterns. Data
regarding the child's behavior at home and at school will also be studied. Only a specialist will be able to accurately detect
whether other problems and/or conditions are resulting in ADHD-like behavioral characteristics.
Interesting links
Diagnostic Criteria for ADHD (ADHD Information Services)
If you do not know how to find a specialist, ask your GP.
When does ADHD start? How long does ADHD last?
According to New Zealand's ADHD Online Support Group, the onset of ADHD usually occurs before the person is 7 years
old. For about 75% of ADHD sufferers, symptoms continue into adulthood. However, levels of hyperactivity tend to decrease
as the person gets older.
click here for source site
  Research Shows A Walk In The Park Improves Attention In Children With ADHD
Main Category: ADHDArticle Date: 16 Oct 2008 - 6:00 PST
For children with Attention Deficit Hyperactivity Disorder
(ADHD) tasks that require concentration such as doing homework or taking a test can be very difficult. A simple, inexpensive
remedy may be a "dose of nature."
A study conducted at the University of Illinois shows that children with ADHD demonstrate
greater attention after a 20-minute walk in a park than after a similar walk in a downtown area or a residential neighborhood.
The study, conducted by child environment and behavior researchers Andrea Faber Taylor and Frances E. Kuo was published
in a recent issue of the Journal of Attention Disorders.
"From our previous research, we knew there might be a link
between spending time in nature and reduced ADHD symptoms," said Faber Taylor. "So to confirm that link we conducted a study
in which we took children on walks in three different settings - one especially "green" and two less "green" - and kept everything
about the walks as similar as possible."
Some children took the "green" walk first; others took it second or last.
After each walk, an experimenter who didn't know which walk the child had been on tested their attention using a standard
neurocognitive test called Digit Span Backwards, in which a series of numbers are said aloud and the child recites them backwards.
It's a test in which practice doesn't improve your score.
"We compared each child's performance to their own performance
on different walks," said Faber Taylor. "And when we compared the scores for the walks in different environments, we found
that after the walk in the park children generally concentrated better than they did after a walk in the downtown area or
the neighborhood area. The greenest space was best at improving attention after exposure."
"What this particular study
tells us is that the physical environment matters," said Kuo. "We don't know what it is about the park, exactly - the greenness
or lack of buildings - that seems to improve attention, but the study tells us that even though everything else was the same
- who the child was with, the levels of noise, the length of time, the time of day, whether the child was on medication -
if we kept everything else the same, we just changed the environment, we still saw a measurable difference in children's symptoms.
And that's completely new. No one has done a study looking at a child in different environments, in a controlled comparison
where everything else is the same."
The sample size was relatively small - only 17 children - mostly because the logistics
were a nightmare to coordinate. "Because we kept everything the same, the children all went to the same park and walked through
the same neighborhood and downtown area. The testing location had to be close by so that there wasn't a lot of lag time between
going for the walk and taking the post-test," said Faber Taylor. "And each child was always paired with the same adult guide
for their walks, and all the children were tested by the same tester."
Kuo said that the variables of the study were
very hard to control. "We started with a much larger sample size. But when we threw out all of the things that could go wrong
- the weather wasn't good one day, the child came late, or came medicated - when we threw out all of those, it left us with
this relatively pure, clean sample to work with."
Faber Taylor added that their confidence in the findings from this
study is bolstered by findings from other studies. "Because we have results from a national study which looked at over 450
children, we can have more confidence that this relationship between natural settings and improved attention is true not just
for the children in this study." She said that the larger study included children from all over the United States, representing
a wide range of ages, different community sizes, and both with and without hyperactivity. "The findings from the national
study give us some confidence that this relationship applies to all children with ADHD."
Kuo emphasized that this
study involved an objective test of attention, not just on children's or parents' impressions.
During the walks, all
of the children were unmedicated -- those of the participants who normally took medications to control their ADHD symptoms
stayed off their medications on the days of the walks. Interestingly, Faber Taylor and Kuo found that a "dose of nature" may
be as helpful -- at least for a while -- as a dose of stimulants. "We calculated the size of the effect in our study and compared
it to the size of effects in a recent medication study," said Faber Taylor, "and we were surprised to see that the dose of
nature had effects the same size or even larger than the dose of medication." What remains to be seen is how long the effects
of a dose of nature last.
"Some of the previous survey research suggests a relationship between children who regularly
play in green spaces and how severe their symptoms are. Children who have regular exposure to green spaces have milder symptoms
overall. So that's hinting that there may be a persistent effect," said Kuo.
She said that while there are hints that
the regular doses of nature work long term - that you can expose a child to the same green outdoor settings day after day
and still get a benefit - the science isn't advanced enough to give parents a strict formula. "We can't say for sure, 'two
hours of outdoor play will get you this many days of good behavior,' but we can say it's worth trying, and we can say that
as little as 20 minutes of outdoor exposure could potentially buy you an afternoon or a couple of hours to get homework done,"
said Kuo. "One reason we believe this is that if the effect were short-lived, we don't think that parents would have so consistently
observed it. But they do. They report it over and over. And they report it independently. So, in the larger study with over
450 kids, we asked 'what's your kid like after watching TV or after playing outside' and none of the parents know what any
of the other parents are telling us, but they overwhelmingly agree."
Faber Taylor believes it would be easy to add
a dose of nature to a child's routine. "I could imagine parents hearing about this research and immediately applying it -
just trying it out - taking their child to the park either when their child's symptoms are exacerbated or as a regular routine.
It's not that hard to incorporate, especially if they have a green backyard or if they can get to a neighborhood park. Again,
we can't say for sure that it would work for any given child - but there's probably very little risk involved in encouraging
your child to play outdoors and seeing if their symptoms improve."
She also says that the benefits of a dose of nature
don't apply just to children with ADHD. "We're all on a continuum of attention so this study has implications for all of us,"
said Taylor. "ADHD is just at the far end of attention functioning, but there're plenty of us who fall somewhere close to
that end of the continuum, and we all experience times when we're mentally fatigued - times when we're less able to focus
and do tasks and get easily distracted. The evidence suggests that natural settings can benefit everyone, even children (and
adults) who have not been diagnosed with ADHD."
Notes: This material is based upon work supported by
the National Urban and Community Forestry Advisory Council, U.S. Forest Service under award No. 00-DG-11244225-354, and the
Cooperative State Research, Education and Extension Service, U.S. Department of Agriculture, under Project No. ILLU-65-0370
Source: Debra Levey Larson University of Illinois at Urbana-Champaign
  Transcendental Meditation Reduces ADHD Symptoms Among Students: New Study
The Transcendental Meditation technique may be an effective
and safe non-pharmaceutical aid for treating ADHD, according to a promising new study published this month in the peer-reviewed
online journal Current Issues in Education.
The pilot study followed a group of middle school students
with ADHD who were meditating twice a day in school. After three months, researchers found over 50 percent reduction in stress
and anxiety and improvements in ADHD symptoms.
Effect exceeds expectations
"The effect was much greater
than we expected," said Sarina J. Grosswald, Ed.D., a George Washington University-trained cognitive learning specialist and
lead researcher on the study. "The children also showed improvements in attention, working memory, organization, and behavior
regulation."
Grosswald said that after the in-school meditation routine began, "teachers reported they were able to
teach more, and students were able to learn more because they were less stressed and anxious."
Stress interferes
with the ability to learn
Prior research shows ADHD children have slower brain development and a reduced ability
to cope with stress. "Stress interferes with the ability to learn - it shuts down the brain," said William Stixrud, Ph.D.,
a Silver Spring, Maryland, clinical neuropsychologist and co-author of the study.
"Medication for ADHD is very effective
for some children, but it is marginally or not effective for others. Even for those children who show improved symptoms with
the medication, the improvement is often insufficient or accompanied by troubling side effects," Stixrud said. "Virtually
everyone finds it difficult to pay attention, organize themselves and get things done when they're under stress. So it stands
to reason that the TM technique which reduces stress and organizes brain function would reduce ADHD symptoms."
While
in some cases a child cannot function without medication, there is growing concern about the health risks and side effects
associated with the common ADHD medications, including mood swings, insomnia, tics, slowed growth, and heart problems. In
2006 the FDA required manufacturers to place warning labels on ADHD medications, listing the potential serious health risks.
These high risks and growing concerns are fueling parents' search for alternatives that may be safer for their kids.
The study was conducted in a private K-12 school for children with language-based learning disabilities. Participation
was restricted to 10 students, ages 11-14, who had pre-existing diagnoses of ADHD. About half of the students were on medication.
The students meditated at school in a group for 10 minutes, morning and afternoon.
To determine the influence of the
TM technique, at the beginning and end of the three-month period, parents, teachers and students completed standard ADHD assessment
inventories measuring stress and anxiety, behavior and social competency, and executive function. Students were also given
a battery of performance tests to measure cognitive functioning.
"The results were quite remarkable"
Andy
and Daryl Schoenbach's daughter was diagnosed with ADHD in second grade. Like most ADHD children she was taking medication.
"The medication helped but had mixed results - she still lost focus, had meltdowns, and the medications affected her sleep
and appetite," said Andy, who lives with Daryl in Washington D.C. "She was not performing close to her potential and we didn't
see the situation improving. So at the end of seventh grade when her doctor recommended increasing the medication, we decided
it was time to take a different course - stopping the medication and using Transcendental Meditation."
"The results
were quite remarkable," Daryl said. "The twice daily meditations smoothed things out, gave her perspective, and enabled her
to be in greater control of her own life when things started falling apart. It took some time, but it gradually changed the
way she handled crises and enabled her to feel confident that she could take on greater challenges - in her own words, 'climb
a mountain.'"
"Everyone noticed the change," Andy added.
Grosswald explained that there is substantial research
showing the effectiveness of the TM technique for reducing stress and anxiety, and improving cognitive functioning among the
general population. "What's significant about these new findings is that among children who have difficulty with focus and
attention, we see the same results. TM doesn't require concentration, controlling the mind or disciplined focus. The fact
that these children are able to do TM, and do it easily shows us that this technique may be particularly well suited for children
with ADHD," she said.
This study was funded by the Abramson Family Foundation and the Institute for Community Enrichment.
A second, recently completed TM-ADHD study with a control group measured brain function using electroencephalography
(EEG). Preliminary data shows that three months practice of the technique resulted in significant positive changes in brain
functioning during visual-motor skills. Changes were specifically seen in the circuitry of the brain associated with attention
and distractibility. After six months TM practice, measurements of distractibility moved into the normal range.
A
third TM-ADHD study, to be funded by a $2 million grant from the David Lynch Foundation, will more fully investigate the effects of the technique on ADHD
and other learning disorders.
----------------------------
Article adapted by Medical News Today from original
press release.
----------------------------
FACT SHEET
Attention Deficit Hyperactivity Disorder
(ADHD)
-- The Center for Disease Control reports that nearly 50 percent of the 4.5 million children (ages 4-17)
in the United States diagnosed with ADHD are on ADHD medication - and the majority of those on medication stay on it in adulthood.
-- The rate of prescriptions for Attention Deficit Hyperactivity Disorder in the U.S. has increasing by a factor of
five since 1991 - with production of ADHD medicines up 2,000 percent in 9 years.
-- The commonly used drugs for ADHD
are stimulants (amphetamines). These drugs can cause persistent and negative side effects, including sleep disturbances, reduced
appetite, weight loss, suppressed growth, and mood disorders. The side effects are frequently treated with additional medications
to manage insomnia or mood swings. Almost none of the medications prescribed for insomnia or mood disturbances are approved
by the Food and Drug Administration (FDA) for use with children.
-- The long-term health effects of ADHD medications
are not fully known, but evidence suggests risks of cardiac disorders and sudden death, liver damage and psychiatric events.
It has also been found that children on long-term medication have significantly higher rates of delinquency, substance use,
and stunted physical growth.
The Transcendental Meditation Technique
-- The Transcendental Meditation
technique is an effortless technique practiced 10-20 minutes twice a day sitting comfortably with the eyes closed.
--
TM is not a religion or philosophy and involves no new beliefs or change in lifestyle.
-- Over 350 peer-reviewed research
studies on the TM technique confirm a range of benefits for mind, body and behavior.
-- Several studies have compared
the effects of different meditation practices and found that Transcendental Meditation provides deeper relaxation and is more
effective at reducing anxiety, depression and hypertension than other forms of meditation and relaxation. In addition, no
other meditation practice shows the widespread coherence throughout all areas the brain that is seen with Transcendental Meditation.
-- The Transcendental Meditation technique is taught in the United States by a non-profit, educational organization.
-- More information can be obtained by calling 888-LEARN-TM or visiting http://www.ADHD-TM.org, http://www.AskTheDoctors.com, or http://www.TMEducation.org.
Ken Chawkin
Maharishi University of Management
http://www.mum.edu
|
 |
|
There is an enormous source of information I just found that
I'd like to offer for you... click here and notice at the bottom of the list there are additional pages to click on for a total of 8 pages of articles concerning
this topic!
kathleen
Symptoms
The principal characteristics
of ADHD are:
- inattention
- hyperactivity
- impulsivity
These symptoms appear early
in a child's life. Because many normal children may have these symptoms, but at a low level, or the symptoms may be caused
by another disorder, it's important that the child receive a thorough examination and appropriate diagnosis by a well-qualified professional.
Symptoms
of ADHD will appear over the course of many months, often with the symptoms of impulsiveness
and hyperactivity preceding those of inattention, which
may not emerge for a year or more.
Different symptoms may appear
in different settings, depending on the demands the situation may pose for the child's self-control. A child who "can't sit still" or is otherwise disruptive will be noticeable in school,
but the inattentive daydreamer may be overlooked.
The impulsive
child who acts before thinking may be considered just a "discipline problem," while
the child who is passive or sluggish may be viewed as merely unmotivated. Yet both may have different types of ADHD.
All children are sometimes
restless, sometimes act without thinking, sometimes daydream the time away. When the child's hyperactivity,
distractibility, poor concentration or impulsivity begin to affect performance in school, social relationships with other children or behavior at home, ADHD may be suspected.
But because the symptoms vary
so much across settings, ADHD is not easy to diagnose. This is especially true when inattentiveness is the primary symptom.
According to the most recent
version of the Diagnostic and Statistical Manual of Mental Disorders2 (DSM-IV-TR), there are 3 patterns of behavior that indicate ADHD.
People with ADHD
may show several signs of being consistently inattentive. They may have a pattern of being
hyperactive and impulsive far more than others of their
age.
Or they
may show all three types of behavior. This means that there are 3 subtypes of ADHD
recognized by professionals.
- predominantly hyperactive-impulsive
type (that doesn't show significant inattention)
- predominantly inattentive type
(that doesn't show significant hyperactive-impulsive behavior)
sometimes called ADD: an outdated term for this entire disorder
- combined type (that displays both inattentive
and hyperactive-impulsive symptoms).
Hyperactivity-Impulsivity
Hyperactive
children always seem to be "on the go" or constantly in motion.
They dash around touching or playing with whatever is in sight, or
talk incessantly. Sitting still at dinner or during a school lesson or story can be a difficult task. They squirm and fidget in their seats or roam around the room. Or they may wiggle their
feet, touch everything, or noisily tap their pencil.
Hyperactive teenagers or adults may feel internally restless. They often report needing
to stay busy and may try to do several things at once.
Impulsive
children seem unable to curb their immediate reactions or think before they
act. They'll often blurt out inappropriate comments, display
their emotions without restraint and act without regard for the later consequences of their conduct.
Their impulsivity may make it hard for them to wait for things
they want or to take their turn in games.
They
may grab a toy from another child or hit when they're upset. Even as teenagers or
adults, they may impulsively choose to do things that have an immediate but small payoff
rather than engage in activities that may take more effort yet provide much greater but delayed rewards.
Some signs of hyperactivity-impulsivity are:
- Feeling restless, often fidgeting with hands or feet, or squirming
while seated
- Running, climbing, or leaving a seat in situations where sitting
or quiet behavior is expected
- Blurting out answers before hearing the whole question
- Having difficulty waiting in line or taking turns.
Inattention
Children who are inattentive have a hard time keeping their minds on any one thing and may get bored with a task after only a few minutes. If they're doing something they really enjoy, they have no
trouble paying attention. But focusing deliberate, conscious attention to organizing and completing
a task or learning something new is difficult.
Homework
is particularly hard for these children. They'll forget to write down an assignment or leave
it at school. They'll forget to bring a book home or bring the
wrong one. The homework, if finally finished, is full of errors and erasures. Homework is often accompanied by frustration for both parent and child.
The
DSM-IV-TR gives these signs of inattention:
- Often becoming easily distracted by irrelevant sights and sounds
- Often failing to pay attention to details and making careless
mistakes
- Rarely following instructions carefully and completely losing
or forgetting things like toys, or pencils, books and tools needed for a task
- Often skipping from one uncompleted activity to another.
Children diagnosed with the
Predominantly Inattentive Type of ADHD are seldom impulsive or hyperactive, yet they have significant problems paying attention. They appear to be:
- daydreaming
- "spacey"
- easily confused
- slow moving
- lethargic
They may have difficulty processing
information as quickly and accurately as other children. When the teacher gives oral or even written instructions, this child has a hard time understanding what he or she is supposed to do and makes frequent mistakes.
Yet the child may sit quietly,
unobtrusively and even appear to be working but not fully attending to or understanding the task and the instructions.
These children don't show
significant problems with impulsivity and overactivity in the
classroom, on the school ground, or at home. They may get along better w/other children than the more impulsive and hyperactive types of ADHD and they
may not have the same sorts of social problems so common with the combined type of ADHD.
So often their problems with
inattention are overlooked. But they need help just as much as children with other types
of ADHD, who cause more obvious problems in the classroom.
Parents should not worry
when their pre-schoolers talk to themselves; in fact, they should encourage it, says Adam Winsler, an associate professor of psychology at George Mason University. His recent study published in Early
Childhood Research Quarterly showed that 5-year-olds do better on motor tasks when they talk to themselves out loud (either spontaneously or when told to do so by an adult) than when they are silent.
"Young children often talk to themselves as they go about their daily activities,
and parents and teachers shouldn't think of this as weird or bad," says Winsler. "On the contrary, they should listen to the private speech of kids. It's a fantastic window into the minds of children."
In
the study, "'Should I let them talk?': Private speech and task performance among preschool children with and without behavior
problems," 78% of the children performed either the same or better on the performance task when speaking to themselves than
when they were silent.
The study also showed that children with behavioral problems
(such as those diagnosed with Attention Deficit Hyperactivity Disorder, or ADHD)
tend to talk to themselves more often than children without signs of behavior problems.
"Given
that kids with behavior concerns need more direction and control from adults, teachers may unnecessarily ask children to be
quiet in classrooms out of fear that such speech coming from difficult-to-manage kids will lead to problem behavior," says
Winsler. "Yet non-disruptive private speech would actually help these children as they develop. Therefore, teacher training
and professional development efforts should suggest that teachers increase their tolerance level for this kind of private
speech."
Winsler says that private speech is very common and perfectly normal among
children between the ages of 2 and 5. As children begin talking to themselves, their communication skills with the outside world improve.
"This is when language comes inside," says Winsler.
"As these two communication processes merge, children use private speech in the transition period. It's a critical period for children, and defines us
as human beings."
Winsler also conducted the first-ever study looking at private
speech in children with autism. He found that high-functioning autistic children talk to themselves often and in the same
ways that non-autistic children do. Talking aloud also improved their performance on tasks.
"Children
with autism have problems with their external social speech, so psychologists assumed that their private speech would also
be impaired," says Winsler. "But this study shows that it is not the case - that autistic children use their private speech
very effectively as a tool to help them with tasks."
----------------------------
Article adapted by Medical
News Today from original press release.
----------------------------
The study, "Private Speech and Executive
Functioning among High-Functioning Children with Autistic Spectrum Disorders," was just published in the Journal of Autism
and Developmental Disabilities.
About George Mason University
George Mason University, located
in the heart of Northern Virginia's technology corridor near Washington, D.C., is an innovative, entrepreneurial institution
with national distinction in a range of academic fields. With strong undergraduate and graduate degree programs in engineering,
information technology, biotechnology and health care, Mason prepares its students to succeed in the work force and meet the
needs of the region and the world. Mason professors conduct groundbreaking research in areas such as cancer, climate change,
information technology and the biosciences, and Mason's Center for the Arts brings world-renowned artists, musicians and actors
to its stage. Its School of Law is recognized by U.S. News & World Report as one of the top 35 law schools in the United
States.
Source: Tara Laskowski
George Mason University
|
 |
 |
 |
|
Disorders that Sometimes Accompany ADHD
Learning Disabilities.
Many children w/ADHD, approximately
20 to 30%, also have a specific learning disability (LD).10 In preschool years, these disabilities include difficulty in understanding certain sounds
or words &/or difficulty in expressing oneself in words.
In school age children, reading
or spelling disabilities, writing disorders & arithmetic disorders may appear. A type of reading disorder, dyslexia, is quite widespread. Reading disabilities affect up to 8% of elementary school children.
Tourette Syndrome.
A very small proportion of
people w/ADHD have a neurological disorder called Tourette syndrome.
People w/Tourette syndrome have various nervous tics &
repetitive mannerisms, such as eye blinks, facial
twitches or grimacing.
Others may clear
their throats frequently, snort, sniff or
bark out words. These behaviors can be controlled w/medication. While very few children
have this syndrome, many of the cases of Tourette syndrome have associated ADHD.
In such cases, both disorders often require treatment that may include medications.
Oppositional Defiant Disorder.
As many as 1/3 to 1/2f of
all children w/ADHD - mostly boys - have another condition, known as oppositional
defiant disorder (ODD).
These children are often:
- defiant
- stubborn
- non-compliant
- have outbursts of temper
- become belligerent
They argue w/adults & refuse to obey.
Conduct Disorder.
About 20 to 40% of ADHD
children may eventually develop conduct disorder (CD), a more serious pattern of antisocial behavior.
These children frequently
lie or steal, fight w/or bully others & are at a real risk of getting into trouble at school or w/the police.
- they violate the basic rights of other people
- are aggressive toward people &/or animals
- destroy property
- break into people's homes
- commit thefts
- carry or use weapons
- engage in vandalism
These children or teens are at greater
risk for substance use experimentation & later dependence & abuse. They need immediate help.
Anxiety & Depression.
Some children w/ADHD
often have co-occurring anxiety or depression. If the anxiety or depression is recognized & treated, the child will be better able to handle the problems that accompany
ADHD.
Conversely, effective treatment
of ADHD can have a positive impact on anxiety as the child is better able to master academic tasks.
Bipolar Disorder.
There are no accurate
statistics on how many children w/ADHD also have bipolar disorder. Differentiating between ADHD & bipolar disorder in childhood can be difficult.
In its classic
form, bipolar disorder is characterized by mood cycling between periods of intense highs & lows. But in children, bipolar disorder often seems to be a rather chronic mood dysregulation w/a mixture of elation, depression & irritability.
Furthermore, there
are some symptoms that can be present both in ADHD & bipolar disorder, such as a high level of energy & a reduced need for sleep. Of the symptoms differentiating children w/ ADHD
from those w/bipolar disorder, elated mood & grandiosity of the bipolar child are distinguishing characteristics.11
The Family & the ADHD Child
Medication can help the ADHD child in everyday life. He or she may be better able to control some
of the behavior problems that have led to trouble w/parents & siblings. But it takes time to undo the frustration,
blame & anger that may have gone on for so long.
Both parents and children
may need special help to develop techniques for managing the patterns of behavior. In such cases, mental health professionals can counsel the child & the family, helping them to develop new skills, attitudes & ways of relating to each other.
In individual counseling, the therapist helps children w/ADHD learn to feel better about
themselves. The therapist can also help them to identify & build on their strengths, cope w/daily problems &
control their attention & aggression.
Sometimes only the child w/ADHD needs counseling support. But in many cases, because the problem affects the family as a whole, the entire family may need help. The therapist assists the family in finding better ways to handle the disruptive behaviors & promote change.
If the child is young, most of the therapist's work is w/the parents, teaching them techniques for coping with & improving
their child's behavior.
Several intervention approaches
are available. Knowing something about the various types of interventions makes it easier for families to choose a therapist
that is right for their needs.
Psychotherapy
works to help people w/ADHD to like & accept themselves
despite their disorder. It doesn't address the symptoms or underlying causes of the disorder. In psychotherapy, patients talk
w/the therapist about upsetting thoughts & feelings, explore self-defeating
patterns of behavior & learn alternative ways to handle their emotions. As they
talk, the therapist tries to help them understand how they can change or better cope w/their disorder.
Behavioral
therapy (BT) helps people develop more effective ways to work on immediate issues. Rather than helping the child understand
his or her feelings & actions, it helps directly in changing their thinking & coping
& thus may lead to changes in behavior.
The support might
be practical assistance, like help in organizing tasks or schoolwork or dealing w/emotionally charged events. Or the support
might be in self-monitoring one's own behavior & giving self-praise or rewards for acting in a desired way such as controlling
anger or thinking before acting.
Social
skills training can also help children learn new behaviors. In social skills training, the therapist discusses &
models appropriate behaviors important in developing & maintaining social relationships, like:
- waiting for a turn
- sharing toys
- asking for help
- responding to teasing
then gives children a
chance to practice.
i.e., a child
might learn to "read" other people's facial expression & tone of voice in order to respond appropriately. Social skills training helps the child to develop better ways to play & work w/other children.
Support
groups help parents connect w/other people who have similar problems & concerns w/their ADHD
children. Members of support groups often meet on a regular basis (such as monthly) to hear
lectures from experts on ADHD, share frustrations & successes & obtain referrals to qualified specialists & information about what works.
There's
strength in numbers & sharing experiences w/others who have similar problems helps people know
that they aren't alone.
Parenting
skills training, offered by therapists or in special classes, gives parents tools & techniques for managing their
child's behavior.
One such technique
is the use of token or point systems for immediately rewarding good behavior or work. Another is the use of "time-out" or isolation to a chair or bedroom when the child becomes too unruly
or out of control.
During time-outs,
the child is removed from the agitating situation & sits alone quietly
for a short time to calm down. Parents may also be taught to give the child "quality time" each day, in which they share a pleasurable or relaxing activity. During this time together, the
parent looks for opportunities to notice & point out what the child does well & praise his or her strengths &
abilities.
This system of rewards &
penalties can be an effective way to modify a child's behavior. The parents (or teacher)
identify a few desirable behaviors that they want to encourage in the child; such as:
- asking for a toy instead of grabbing it
- completing a simple task
The child is told exactly
what's expected in order to earn the reward. The child receives the reward when he performs the desired behavior & a mild
penalty when he doesn't. A reward can be small, perhaps a token that can be exchanged for special privileges, but it should
be something the child wants & is eager to earn.
The penalty might be removal
of a token or a brief time-out. Make an effort to find your child being good. The goal,
over time, is to help children learn to control their own behavior & to choose the more desired behavior. The technique
works well w/all children, although children w/ADHD may need more frequent rewards.
In addition, parents may learn
to structure situations in ways that will allow their child to succeed. This may include
allowing only one or two playmates at a time, so that their child doesn't get overstimulated.
Or if their child has trouble
completing tasks, they may learn to help the child divide a large task into small steps, then praise the child as each step
is completed.
Regardless of the specific
technique parents may use to modify their child's behavior, some general principles appear to be useful for most children
w/ADHD. These include:
- providing more frequent & immediate feedback (including rewards & punishment)
- setting up more structure in advance of potential problem situations
- providing greater supervision & encouragement to children
w/ADHD in relatively unrewarding or tedious situations
Parents may also learn to
use stress management methods, such as meditation, relaxation techniques & exercise, to increase
their own tolerance for frustration so that they can respond more calmly
to their child's behavior.
Some Simple Behavioral Interventions
Children with ADHD may need help in organizing. Therefore:
- Schedule. Have the same routine
every day, from wake-up time to bedtime. The schedule should include homework time and playtime (including outdoor recreation
and indoor activities such as computer games). Have the schedule on the refrigerator or a bulletin board in the kitchen. If
a schedule change must be made, make it as far in advance as possible.
- Organize needed everyday items.
Have a place for everything and keep everything in its place. This includes clothing, backpacks, and school supplies.
- Use homework and notebook organizers.
Stress the importance of writing down assignments and bringing home needed books.
Children with ADHD need consistent rules that they can understand
and follow. If rules are followed, give small rewards. Children with ADHD often receive, and expect, criticism. Look for good
behavior and praise it.
Your ADHD Child & School
You
are your child's best advocate. To be a good advocate for your child, learn as much as you can about ADHD & how it affects your child at home, in school & in social situations.
If your child has shown symptoms
of ADHD from an early age & has been evaluated, diagnosed & treated w/either behavior
modification or medication or a combination of both, when your child enters the school system, let
his or her teachers know.
They'll be better prepared
to help the child come into this new world away from home.
If your child enters school
& experiences difficulties that lead you to suspect that he or she has ADHD, you can
either seek the services of an outside professional or you can ask the
local school district to conduct an evaluation.
Some parents prefer to go
to a professional of their own choice. But it's the school's obligation to evaluate children
that they suspect have ADHD or some other disability that's affecting not only their academic
work but their interactions w/classmates & teachers.
If you feel that your child
has ADHD & isn't learning in school as he or she should, you should find out just who
in the school system you should contact. Your child's teacher should be able to help you w/this information.
Then you can request, in writing, that the school system evaluate your child. The letter should include the date, your
& your child's names & the reason for requesting an evaluation. Keep a copy of the letter in your own files.
Until the last few years,
many school systems were reluctant to evaluate a child w/ADHD. But recent laws have made
clear the school's obligation to the child suspected of having ADHD that's affecting adversely
his or her performance in school.
If the school persists in
refusing to evaluate your child, you can either get a private evaluation or enlist some help in negotiating w/the school.
Help is often as close as a local parent group.
Each state has a Parent Training & Information (PTI) center as well as a Protection & Advocacy (P&A) agency. (For info on the law & on the PTI & P&A, see the section on support groups & organizations
at the end of this document.)
Once your child has been diagnosed
w/ADHD & qualifies for special education services,
the school, working w/you, must assess the child's strengths & weaknesses & design an Individualized
Educational Program (IEP).
You should be able periodically
to review & approve your child's IEP. Each school year brings a new teacher & new schoolwork, a transition that can
be quite difficult for the child w/ADHD. Your child needs lots of support & encouragement
at this time.
Never forget the cardinal
rule: you're your child's best advocate.
Following is a list of organizations that may be able to provide
additional information and/or assistance about mental health topics:
Attention Deficit Hyperactivity Disorder
Ctr. for Mental Health Services
Substance Abuse & Mental Health Services Admin.
Rm 12-105 Parklawn Building
Rockville, MD 20857
Phone: 301-443-8956
Fax: 301-443-9050
URL: http://www.samhsa.gov/
National Institute of Mental Health
Office of Communications
6001 Executive Blvd., Rm. 8184, MSC 9663
Bethesda, MD 20892-9663
Phone: 301-443-4513
Fax:
301-443-4279
TollFree: 1-866-615-NIMH (6464)
TTY: 301-443-8431
Email: nimhinfo@nih.gov
URL: http://www.nimh.nih.gov
US Dept. of Education
400
Maryland Avenue, SW
Washington, DC, 20202
Fax: (202) 401-0689
TollFree: 1-800-USA-LEARN
TTY: 1-800-437-0833
Email:
customerservice@inet.ed.gov
URL: http://www.ed.gov/index.jhtml
American Academy of Child & Adolescent
Psychiatry (AACAP)
3615 Wisconsin Avenue, N.W.
Washington, DC, 20016-3007
Phone: (202) 966-7300
Fax: (202)
966-2891
URL: http://www.aacap.org/index.htm
American Psychiatric Assoc.
(APA)
1000 Wilson Boulevard, Suite 1825
Arlington, VA 22209-3901
Phone: 703-907-7300
URL: http://www.psych.org/index.cfm
American Psychological Assoc.
750 1st Street, NE
Washington, DC 20002-4242
Phone: 202-336-5510
TollFree: 1-800-374-2721
URL: http://www.apa.org
Attention Deficit Disorder Assoc.
(ADDA)
P.O. Box 543
Pottstown, PA 19464
Phone: (484) 945-2101
Fax: (610) 970-7520
Email: mail@add.org
URL:
http://www.add.org
Attention Deficit Information Network
(AD-IN)
58 Prince Street
Needham, MA 02492
Phone: 781-455-9895
Email: adin@gis.net
URL:
http://www.addinfonetwork.com/
Children & Adults w/Attention
- Deficit Hyperactivity
Disorder (CHADD)
8181 Professional Place, Suite 150
Landover, MD 20785
Phone: 301-306-7070
Fax: 301-306-7090
TollFree: 800-233-4050
URL: http://www.chadd.org/
Learning Disabilities Assoc. of America
4156 Library Road
Pittsburgh, PA 15234-1349
Phone: 412-341-1515
URL: http://www.ldanatl.org/
National Ctr. for Learning Disabilities
381 Park Avenue South Ste. 1401
New York, NY 10016
Phone: 212-545-7510
Fax: 212-545-9665
TollFree: 888-575-7373
URL:
http://www.ncld.org/research/index.cfm
National Information Ctr. for Children
& Youth w/ Disabilities
(NICHCY)
PO Box 1492
Washington, DC, 20013
Fax: 202-884-8441
TollFree: 800-695-0285
Email: nichcy@aed.org
URL:
http://www.nichcy.org/
Homework Help for the Attention Deficit Disorder Child
- By Jeannine Virtue
Does the homework battle so typical with your hyperactive
or A.D.D. child have you at the end of your rope? Relax. We have some tried-and-try ADHD information that should get your
A.D.D. child on the right homework path.
The hyperactive or A.D.D. child especially needs consistency, a work place
free of distractions, solid encouragement and praise - along with established consequences if the positive homework tips fail.
Establish a Set Homework Routine:
Because the A.D.D. child functions best in a consistent environment, homework
should be done in the same place, at the same time and for a set amount of time every day.
Work with your child to
develop that routine. Some Attention Deficit and hyperactive children work best immediately after school while others need
an hour or two to settle down before jumping back into studies.
To help the A.D.D. child better focus, the work area
should be free of distractions, such as televisions, video games, music and other people. The kitchen table might not be the
best place if there is too much activity in that room. The bedroom can offer distractions if the television or stereo have
a way of "turning themselves on" when you are not there to monitor.
Mandatory Homework Time:
We are strong
proponents of establishing an allotted amount of homework time on school days. This set amount of time gives consistency to
the hyperactive or A.D.D. child and discourages rushing through homework.
Talk with your child's teachers about the
average recommended homework time for the child's grade level. In general, elementary school children should spend about 30
minutes each night on homework. Middle school and high school students should spend about one hour on homework.
If
the child does not have homework that evening or they finish before the allotted time, the child can read until their mandatory
homework time is over.
"Chunking" and Scheduled Breaks:
The hyperactive and A.D.D. child often experiences difficulty
with long-range tasks. "Chunking" homework for the hyperactive or A.D.D. child helps break the homework task into smaller,
more manageable pieces.
You can break a 20-problem math assignment into four chunks of five problems each, with a
small break in between chunks. If using the mandatory homework time schedule, set a kitchen timer to ring every five to 15
minutes, depending on the child's attention span. At every break, give your hyperactive or A.D.D. child a few minutes to move
around or grab a snack to refocus their attention.
Rewards/Consequences:
As with any parenting issue, rewarding
good behavior and disciplining poor behavior motivates kids toward good behavior. The A.D.D. child needs all the rewards they
can get, along with firm and consistent consequences.
A “homework contract” is an effective motivator for
the A.D.D. and an especially valuable tool to encourage the A.D.D. child to accept responsibility for their work.
The
homework contract clearly states that when the homework is completed, the child will earn a reward. The contract also clearly
outlines consequences for not completing homework.
You can offer daily modest rewards like earning time to play Gameboy,
the right to choose a favorite dinner or a modest treat or special privilege. Or, you can develop a point system for larger
weekly rewards. You can give out one point for every night of completed homework for the child to cash in for a trip to the
zoo after earning five points, for instance.
Effective consequences for not completing homework are losing phone, computer,
stereo and television privileges for the evening. To add a little more discomfort to the situation, have the child stay inside
for the evening without friends.
It is important that you remain calm, firm and consistent on nights when Attention
Deficit Disorder child decides to get into a power struggle over homework. It may take a couple consequence days before the
child realizes that completing homework makes for a better night than not doing homework.
It is also important that
you reward for effort and not just grades for the A.D.D. child. The goal is to develop a solid homework habit. With a homework
habit established, better grades will automatically follow.
Don't forget to offer the intangible rewards of smiles
and praise when your child puts the effort into completing his homework. A "way to go" goes a long way in positive reinforcement
for Attention Deficit Disorder children.
Additional Homework ADHD Information:
_ Using an assignment book for
the A.D.D. child helps parents keep track of the child's daily and weekly homework. If the teacher does not use an assignment
book, develop a system with the teacher so you know the child's homework assignments.
_ If the A.D.D. child insist
on heavy parental homework help, require that the child attempt problems at least twice before asking for homework help. They
may need homework help, but make sure he puts a genuine effort into solving the problem first.
_ Attention Deficit
and hyperactive children may not be able to receive "A"s on every homework and school assignment. Instead of getting hung
up on the traditional grading scale, give you’re A.D.D. child an "A" for effort.
Increased Risk For Eating Disorders Found In Adolescent Girls With ADHD
Girls with attention deficit hyperactivity disorder stand a substantially greater risk
of developing eating disorders in adolescence than girls without ADHD, a new study has found.
"Adolescent girls with
ADHD frequently develop body-image dissatisfaction and may go through repeating cycles of binge eating and purging behaviors
that are common in bulimia nervosa," said University of Virginia psychologist Amori Yee Mikami, who led the study.
The
findings appear in the current issue of the Journal of Abnormal Psychology.
ADHD is a disorder that affects
about 5 percent of school-age children, and three times more boys than girls. Symptoms include a short attention span, poor
organization, excessive talking, disruptive and aggressive behavior, restlessness and irritability. Many children with ADHD
suffer through a range of problems, from poor grades to poor relations with parents and teachers, and more than half have
serious problems making friends.
Because the disorder is far more common in boys, researchers are still learning its
long-term effects on girls.
"Our finding suggests that girls may develop a broader range of problems in adolescence
than their male counterparts," Mikami said. "They may be at risk for eating problems, which are a female-relevant domain of
impairment. We know that eating disorders occur 10 times more often in girls than boys."
Additionally, Mikami noted
that because ADHD is more common in boys, many girls with the disorder may go undiagnosed and untreated.
"Girls with
ADHD may be more at risk of developing eating problems as adolescents because they already have impulsive behaviors that can
set them apart from their peers," Mikami said. "As they get older, their impulsivity may make it difficult for them to maintain
healthy eating and a healthy weight, resulting in self-consciousness about their body image and the binging and purging symptoms."
The study was conducted with an ethnically diverse sample of 228 girls in the San Francisco Bay area; 140 who had
been diagnosed with ADHD and 88 matched comparison girls without ADHD. They were first assessed between the ages of 6 and
12 and again five years later.
Girls with the "combined type" of ADHD (those with both inattention and hyperactivity/impulsivity)
were most likely to have adolescent bulimia nervosa symptoms, relative to girls with the "inattentive type" of ADHD (those
with inattention only) and girls without ADHD. Girls with both types of ADHD were more likely to be overweight, to have experienced
harsh/critical parenting in childhood, and to have been peer-rejected than girls without ADHD. Mikami said she believes these
factors could contribute to the bulimia nervosa symptoms.
"An additional concern is that stimulant medications used
to treat ADHD have a side effect of appetite suppression, creating a risk that overweight girls could abuse these medicines
to encourage weight loss, though we have not yet investigated that possibility," Mikami said.
She warned parents and
teachers to be aware that adolescent girls with ADHD may develop an array of female-relevant symptoms beyond the standard
ADHD symptoms, to include eating disorders, depression and anxiety.
----------------------------
Article
adapted by Medical News Today from original press release.
----------------------------
Source: Amori Mikami
University of Virginia
source site: click here
|
|
 |
 |
 |
|
|
|